All I did was try to sit on a bed. But sharp pain on my right knee had me crumpled on the floor in an instant. Somewhere between walking toward the bed and turning my feet to sit down, I had strained my medial collateral ligament (MCL).
To fix it, I went to the same orthopedic surgeon who reconstructed my anterior cruciate ligament (ACL) a decade ago. He said I just needed some physical therapy, which I dutifully did at his clinic and at home.
But the pain worsened; it was painful to go down the stairs or even do simple pivoting movements, like going somewhere to sit.
My husband’s gymnast cousin recommended I see Dr. Isagani Leal, a specialist in nonsurgical management of musculoskeletal pain and sports injuries. His clinic lobby at the Philippine Center for Musculoskeletal Medicine at 33 West Ave., West Triangle, Quezon City, was packed with both geriatric- and athletic-looking patients.
After a short discussion, an ultrasound and an X-ray, Dr. Leal said my right knee was overused; having compensated for the reconstructed ACL on my left knee for a decade, my right MCL was strained. I also had painful bone spurs under my right illiotibial band from my years of martial arts and running.
Leal explained that this was why exercising in my condition only added to the pain. He recommended we do a platelet-rich plasma (PRP) procedure.
Repair and recovery
Growth factors and cytokines that our platelets naturally produce reportedly stimulate bone and tissue healing. In joints like knees, blood supply is usually low, so injecting one’s own PRP into the area advances repair and recovery, as the area cannot heal by itself.
Since 2009, Leal has been administering PRPs in the country.
Erwin Benedict Valencia, DPT, director of medical and performance services, Baseball New Zealand, is the former rehabilitation director of the Pittsburgh Pirates, a major league baseball club and the first Filipino to lead the medical staff of a major global sports organization. On PRP, he said, “There is no current evidence regarding the true efficacy of PRP, but it seems to be an option that people are exploring nowadays.”
From the 1970s, PRP has been used in other medical fields, but people have become more aware of it due to stories of how it has quickly and effectively “healed” famous athletes like Tiger Woods.
“The UST Tigers’ Jeric Teng developed multiple shoulder injuries. They opted for a nonsurgical approach through PRP. He was able to return to play after five weeks,” said Leal.
His PRP patients list include PBA players and Gilas Team members Ranidel de Ocampo (torn calf muscle) and Jayson Castro (strained tendon); boxers Mark Anthony Barriga (torn rotator cuff) and Charlie Suarez; and volleyball players Gretchen Ho and Angeli Tabaquero, among others. “Most of the Azkals Team and our national athletes have also been treated with PRP for their injuries,” he said.
The content of our blood changes in composition; this variability does not allow scientists to compare outcomes.
So how sure are we that the sample we get will work? “There are four factors to consider for the PRP treatment to be successful. First, proper patient or case selection. Cases should be classified: complete ACL tears and Achilles tendon full thickness tears are not amenable to PRP.
“Second, proper preparation of PRP. Volume and concentration of PRP is adjusted depending on the location, degree of the injury and type of soft tissue, which is usually identified and quantified through the use of musculoskeletal diagnostic ultrasound and diagnoscopy. It is the first and the only one in the country,” said Leal.
Exact location
“Third, PRP should be injected at the exact location of the injury. It is done through the use of ultrasound, fluoroscopic X-ray or diagnoscopic-guided injection. Before the injection, simulation of acute injury should be done if the injury is chronic so that PRP will adhere to the source of bleeding and will not shed off to other places.
“Fourth, rehabilitation is also important. The injured part must be immobilized for two to eight weeks depending on the injury. While immobilized, patient may undergo cold laser therapy to induce the healing process. If these four factors are properly implemented, there is a higher chance of success.
“So far, I have not encountered a failure in PRP since from the very beginning, we already know which cases have good prognoses and we disregard and refer for surgery those that will not respond to PRP. Usually, PRP fails if the patient does not cooperate or does not follow the protocol, especially in the rehabilitation phase,” he said.
On Oct. 19, 2012, I underwent the outpatient procedure. Dr. Leal’s associate tried to draw blood from my arm but since I have thin, collapsible veins they had trouble with this. I had to go to the laboratory clinic beside their office as their medtech had the butterfly (thinner) needle needed for people like me.
Once they drew a bunch of test tubes’ worth of my blood, they spun this in a centrifuge to isolate the platelet-rich plasma from the rest of my blood. Dr. Leal had a number of visiting students present at my procedure, so it was a bit embarrassing to grimace (okay, more like howl) through the momentary burning feeling as he injected the PRP into my knee, aided by ultrasound. It was a one time, big time “Ouch!”
Afterward, I was given a pain reliever (Tromil) and a month’s worth of collagen pills. “Tendon has 95-percent collagen, which provides elasticity and flexibility of soft tissues,” said Leal.
Dr. Leal’s clinic also lent me an immobilizer for right after the procedure, as for two weeks I wasn’t allowed to bend my knee. Two days after the procedure, my knee couldn’t get wet, too. During this time, taking a shower, sitting on a toilet and riding in vehicles were challenging. Having had a similar recovery experience during my ACL reconstruction before helped me to prepare and plan ahead for these times.
Laser therapy
Three days after the procedure, I had laser therapy every other day for two weeks. This entailed lying still for 20 minutes while a red beam of light painlessly zeroed in on my knee.
How does cold laser therapy work and what is it for? Leal explained, “Cold laser works in the same way that you want to bring two rubber bands together. In order to adhere, you have to apply heat to both ends of the bands to loosen up the molecular bonding to make them melt and then adhere.”
Valencia believes differently: “Lasers, as with many electrotherapy modalities, still lack evidence of efficacy as a treatment option for many sports injuries, despite being pushed in the market heavily,” he said.
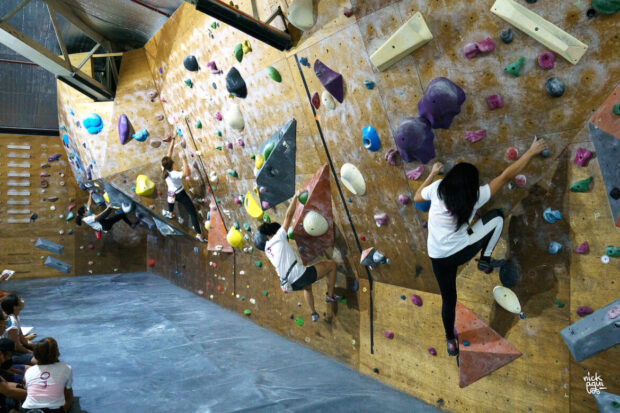
After laser therapy, I had to do seven sessions of virtual rehab for another two weeks using a virtual rehab machine called BalPro. It is a mobility test and evaluation equipment for rehabilitation exercise. A diagnosis is done before rehabilitation training.
Then, I played a video game by shifting my weight and bending my knees at various angles and depths to “grab” fruits spread apart onscreen. Weight sensors detected the shifting of my weight, while tilt sensors measured the angle of my knee bends. The computer measured my leg muscle strength and balance by calculating weight differences between the left and right sides of my body, and my legs’ range of motion. Through the repetitive motions, muscular power of the lower limbs is supposedly strengthened.
But how effective is BalPro vs other forms of physical rehab? Valencia said, “There could be use for BalPro in a rehabilitation and sports setting, but it merely serves as an expensive piece of equipment in a program that could readily be done by a qualified practitioner that thinks beyond modalities and gets creative in his/her rehab program.”
It was a bit uncomfortable at first to play the game, having been immobilized for two weeks, but my natural competitive spirit worked well to egg me on to do better at each level of the game. It was a fun way to push myself to do more.
I was given the go-signal to start working out again right after an evaluation, so I was back to regular programming after only a month. I started the Tracy Anderson Method (TAM) in November 2012, which entails an hour’s worth of intense cardio and matwork, six days a week.
I was surprised to be able to do many deep squats, high kicks and lots of jumping and pivoting, pain-free! PRP may not be for everyone, but it’s now a little over a year after my PRP procedure, and I’m glad I went through this alternative procedure as I’m still actively, happily doing TAM.