A 72-year-old long-time patient of ours complained recently of increasing forgetfulness, which seemed to be getting worse over time.
It started with remembering names. He couldn’t remember names of new acquaintances, so he had to write them down and read the names on the list from time to time so he could remember them. Then many times, he would be put in an embarrassing situation when there would be a lag of a few seconds before he could remember the names of even relatives and longtime friends.
Finding things he has misplaced is a regular challenge to the entire household—car keys, reading glasses, wallet, pill box and envelopes of newly withdrawn cash from the bank.
He can still clearly remember memories of his childhood—the complete name of his best friend in elementary and the places they frequented, his favorite teacher in school and what he liked about her, the first day he wore long pants—but he has difficulty remembering what he had for dinner the previous day or what he and his friend discussed on the phone recently. His long-term memory was still very good, but his short-term memory not as well.
Otherwise, he still functions normally. He drives his daughters to work, does the groceries, and plays cards and mahjong very well.
“Am I developing Alzheimer’s disease?” he asked us. He seemed to be more worried about it than his clogged heart arteries, which cause his heart to go into heart failure from time to time.
“No, it doesn’t look like you have Alzheimer’s,” we assured him, “but you do have signs of cognitive or mental decline, which at your age and with all the cardiovascular risk factors you have—hypertension, diabetes, elevated cholesterol and previous history of smoking—is still par for the course.”
Not necessarily Alzheimer’s
So an age-related deterioration in the brain’s functions and capacity is not necessarily equivalent to Alzheimer’s disease. Although it’s ideal to closely monitor these patients, since mild cognitive impairment (MCI) could be a transition zone between age-related mental function deterioration and Alzheimer’s disease.
Our brain’s various mental functions subtly decline with age. Some experts tell us that the brain’s capacity for memory, reasoning and comprehension skills—all of which are labeled as cognitive function—can actually start to decline from age 45, or at least, much earlier than the age of 60 or 70, as previously thought.
In his extensive review of literature published several years ago in the Neurobiology of Aging Journal, Dr. Timothy Salthouse and his group from the Department of Psychology, University of Virginia, USA, showed that cross-sectional comparisons from 18 to 60 years of age have consistently revealed that as one ages, there are associated decreasing levels of cognitive performance, which seem to accelerate in some as early as 45 years of age.
The general assertions before Dr. Salthouse’s publication was that cognitive decline occurred later in life. According to Aartsen et al., “Cognitive decline may begin after midlife, but most often occurs at higher ages (70 or higher).” Albert and Heaton wrote that “… relatively little decline in performance occurs until people are about 50 years old.”
Plasman, et al., believed that “cognitive abilities generally remain stable throughout adult life until around age 60.” Ronnlund et al. wrote in their thesis that “no or little drop in performance (occur) before age 55 …” Schaie et al., asserted that “most abilities tend to peak in early midlife, plateau until the late 50s or 60s, and then show decline, initially at a slow pace, but accelerating as the late 70s are reached.”
Although Dr. Salthouse’s findings have been challenged by other authors and researchers, we believe he could be correct with this assumption. The reason there may be some age-cognitive function discrepancy in other studies is that the decline in memory and other mental skills may be masked by the increase in experience, insights, and possibly enhanced grace and confidence that also come with age.
Most productive years
Theoretically, the brain cells may be deteriorating as one ages, but this is more than compensated for by what one has gained in his or her more vast experience in life and the wisdom that comes with it. This is the reason why some claim that one’s most productive years are between the ages of 55 and 75.
A justice of the Supreme Court nearing the retirement age of 70 may no longer remember all the details of a case, but his or her erudition of the law, experience-based wisdom and good judgment are more important traits in the dispensation of justice.
A practicing physician in his late 70s may no longer know the details of how a new drug works in the body, but his so-called “clinical eye” is sharper than ever and can intuitively make him discern what might be ailing the patient the moment he or she walks in.
An elderly scientist may not fare as well as his colleagues 30 years his junior in memory skills, but he would rate higher in analytical or other so-called higher-learning skills.
So, when should one worry about one’s deteriorating memory? When can we say it’s not only age-related, and still par for the course for those with high blood pressure, diabetes and other risk factors?
There’s reason to worry if the decline in memory and other mental functions already interferes with one’s work. In the case of our patient, he’s still perfectly functional and able to do most of the things he’s supposed to do. He just needs to be a little more organized in the way he does things, like leaving his car keys, wallets, reading glasses, etc. in the same place so he knows exactly where to get them when he needs them; regularly writing down notes in his journal of the things he did, and people he met; writing on Post-Its important appointments and instructions; and other simple means to assist his failing memory.
More serious problems
It’s true that initially, it may be difficult to distinguish the memory loss pattern of age-related mental decline from Alzheimer’s disease. Only the short-term memory may also be affected in early Alzheimer’s disease, and their long-term memory may still be intact, which is pretty much the same in age-related memory decline.
When we say there’s already Alzheimer’s disease or other types of dementia, it already indicates a more serious brain problem that interferes with one’s ability to think, understand, communicate, interact with others and perform activities of daily living.
There is usually a deterioration in most if not all mental processes such as thinking, reasoning, learning, problem solving, memory, language and speech. Because of the interference in one’s behavioral interactions, one’s ability to navigate social functions is also seriously impaired in dementia.
Although it may present very mildly at the start, just like any age-related memory decline, Alzheimer’s disease and other types of dementia are generally rapidly progressive and may soon be accompanied by behavioral and personality changes. In short, one with Alzheimer’s or dementia can no longer function well, and may no longer be able to take care of oneself. He or she has to be assisted.
Prevention
Why is it important to realize that significant mental function decline can occur as early as 45 years of age? All interventions now at preventing mental decline, whether it’s lifestyle change (diet, physical and mental exercises) or pharmacological (brain-cell transmission enhancing drugs), are usually focused on people in their 60s or 70s. It might already be too late by then for some people because irreversible changes may have already happened in the brain.
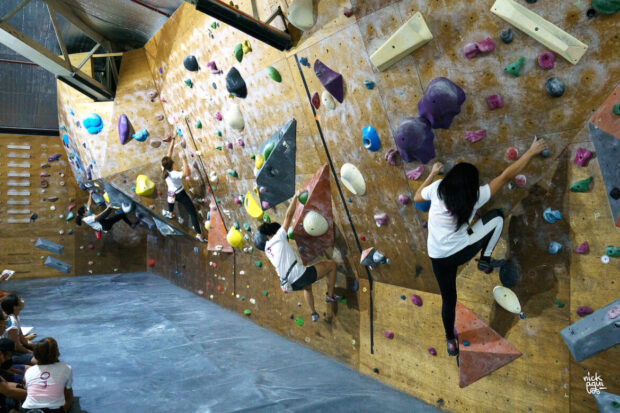
Interventions at prevention should be started much earlier, particularly in those with risk factors such as strong family history of dementia, atherosclerotic cardiovascular disease (buildup of plaques in the arteries of the body), diabetes and hypertension, unhealthy lifestyle (diet rich in processed foods, sedentariness), smoking and excessive alcohol intake, obesity and obstructive sleep apnea.
Many young adults already have several of these risk factors. The earlier control measures are started, the better the chances of mitigating the early decline in their mental function, and the better their chances of enjoying life to the fullest even in their sunset years.