The world is once again in the grip of a pandemic. The last severe influenza pandemic in 1918 spread worldwide until 1919, infecting a third of the world’s population (about 500 million) and killing at least 50 million people.
Hospitals worldwide were overwhelmed. With no vaccine and antibiotics, control efforts by government agencies around the world were, just like today, limited to nonpharmaceutical interventions such as quarantine, isolation, good personal hygiene, use of disinfectants and social distancing.
More than a century has passed since the 1918 influenza pandemic. Are we now prepared for a full-blown pandemic? Uncharted territory
“Handling and controlling pandemics is really uncharted territory even for infectious diseases specialists, because the last pandemic happened more than a century ago,” said Inquirer columnist and cardiologist Raphael R. Castillo. “It killed around 50 million people. So, with the current COVID-19 pandemic afflicting more than 100,000 and killing more than 4,000, we dread to imagine that we may just be in the ‘introductory’ phase of the pandemic.”
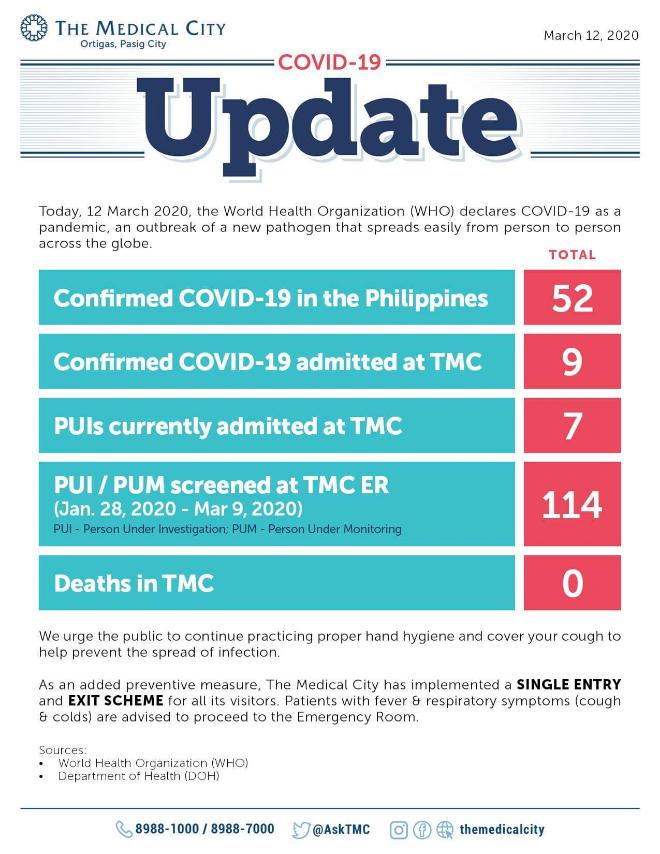
Hospitals like The Medical City (TMC), however, have an Epidemic Rapid Response Team (ERRT) to address the pandemic in a local setting. There’s a Fever Clinic; single entry and exit were implemented for patients, visitors and guests at the foyer to ensure everyone gets screened before entering the medical facilities.
The ERRT ensures proper training of all healthcare providers handling persons under investigation (PUI) and confirmed COVID-19 patients, said Anne Malolos de Aquino, AVP for TMC marketing and communications. “The Medical City follows international protocols in dealing with the outbreak. Protocols from the World Health Organization (WHO) and Center for Disease Control (CDC) are put in place as well as locally implemented protocols coming from the Department of Health and the Philippine Society for Microbiology and Infectious Diseases.”
Mock drills
Makati Medical Center (MMC) also has its Pandemic Influenza and Emerging Disease Response (Peder) regularly activated and tested, even for mock drills, said Arlyn L. Songco, MMC VP for marketing and sales services.
Despite the stringent screening and isolation imposed by hospitals, nearly everyone has been avoiding going to the hospital for fear of contracting the virus.
De Aquino, however, said that the prevention of transmission is highly dependent on how people practice hygiene and conduct social distancing.
“If one needs to be in a hospital for a required procedure, the benefit of going to the hospital at this time should outweigh the risk of possible exposure to any communicable disease, COVID-19 or not,” said Songco.“Our best hope, really, is to not allow the natural progression of the COVID-19 pandemic by containing it as best as we can, to flatten the rapid steep curve of contagion spread. That’s why lockdown of specific areas may be a bitter pill that we have no choice but to swallow,” Castillo said.
Social distancing
Social distancing is critical to prevent the pandemic from going out of hand. So while some people proudly announce they will not allow fear to control their lives and vow to continue living life prepandemic-style, it is everyone’s moral responsibility to limit social interaction. By doing so, we also limit the chance of the virus spreading.
“There is a lot of known and shared information about COVID-19, but there are more unknowns about it at this time. The algorithm/process for screening has changed several times from its initial announcement,” Songco said.
Castillo said that practically all hospitals have an infectious disease emergency committee. Hospitals, he said, “conduct ‘generic’ training for hospital personnel on infection control and prevention, but nothing commensurate to the magnitude of the problem posed by COVID-19.”“Most hospitals know, in theory, what to do. Protocols are in place on how to handle suspected cases, but knowing what to do and being able to do what you know should be done are two different things which may not necessarily go hand in hand,” Castillo said.
Best bet
“For example, we still have limited PPE (personal protective equipment) for front-line doctors and nurses, and that includes even face masks in some hospitals; a limited number of diagnostic kits, so it may take several days to confirm the diagnosis; and limited ventilators to support breathing for those patients who can no longer breathe on their own.”
Songco said the MMC keeps safe inventory levels of critical supplies, and these are monitored daily. “As with the previous epidemics, SARS, MERS-CoV and H1N1, MMC is prepared to handle outbreaks. Systems, policies, protocols and processes are already in place, which are regularly activated and tested,” she said.
Castillo, however, thinks the world is not ready for a full-blown pandemic.
“It’s not ‘crying wolf’ to predict that there will be a breakdown of most countries’ healthcare systems, not only ours, in the event of a full-blown pandemic, so our best bet is containment at this point, and risk mitigation,” he said.
Maximum capacity
Castillo added that most tertiary and even secondary hospitals have isolation rooms and wards. Government hospitals are mandated not to admit private-room patients in anticipation of the increasing number of COVID-19 admissions.
There may be enough rooms and beds for now, he said, “but unless the big hospitals allocate more rooms as properly equipped isolation rooms with enough PPE for its front-line personnel, we’ll soon reach maximum capacity, and to think that the pandemic has just started.”
The situation is that serious.
“A month ago, I didn’t expect COVID-19 to hit the pandemic threshold. The current COVID-19 trajectory indicates a gloomy outcome. But a calm, well-calibrated all-of-society response can still avert a national and global catastrophe,” Castillo said.
“We should all be part of the solution by strictly following expert recommendations on risk containment… Once the pandemic crosses the Rubicon, which is no longer an entirely remote scenario judging from the rate of spread of this contagion, there’s no turning back, and only God’s mercy can allow us to find our way back to normalcy,” he added. INQ